Quaderns de Psicologia | 2023, Vol. 25, Nro. 2, e1867 | ISNN: 0211-3481 | 
 https://doi.org/10.5565/rev/qpsicologia.1867
https://doi.org/10.5565/rev/qpsicologia.1867

Ethical principles in psychotherapy within a broad psychological and medical deontological framework: An international comparison
Principios éticos en psicoterapia dentro de un amplio marco deontológico psicológico y médico: una comparación internacional
Miguel Ricou
Porto University
Ana N. Silva
Universidade de Lisboa
David D. Neto
ISPA – Instituto Universitário/ APPsyCI- Applied Psychology Research Center Capabilities & Inclusion
Sílvia Marina
Porto University
Abstract
Awareness of ethics codes and professional guidelines is crucial to a professional role in psychotherapy practice. Psychotherapy practice is increasingly heterogeneous, and there is much discussion about their effectiveness for clients. In some countries, psychotherapy is an autonomous profession. In others, is part of the professional features of psychologists and psychiatrists, and it is possible to find other health professionals working as psychotherapists in some countries. Considering that ethical principles are central to the performance of a profession, we intend to find connections between the ethical principles for psychotherapists and psychologists or psychiatrists. A critical review was done to promote an integrative vision of ethics codes in psychotherapy. Content analysis of the ethics codes in psychotherapy was performed. Confidentiality, competence, and integrity were the principles more frequently found. Psychotherapists seem to have a major concern with interpersonal relationships and are less linked to social responsibility.
Keywords: Psychotherapy; Psychology; Codes of Ethics; Professional Practice
Resumen
El conocimiento de los códigos éticos y las directrices profesionales es crucial para desempeñar un papel profesional en la práctica de la psicoterapia. La práctica de la psicoterapia es cada vez más heterogénea y se discute mucho sobre su eficacia para los clientes. En algunos países, la psicoterapia es una profesión autónoma. En otros forma parte de las características profesionales de psicólogos y psiquiatras, y es posible encontrar a otros profesionales de la salud trabajando como psicoterapeutas en algunos países. Considerando que los principios éticos son centrales para el desempeño de una profesión, pretendemos encontrar conexiones entre los principios éticos para psicoterapeutas y psicólogos o psiquiatras. Se realizó una revisión crítica para promover una visión integradora de los códigos de ética en psicoterapia. Se realizó un análisis de contenido de los códigos de ética en psicoterapia. La confidencialidad, la competencia y la integridad fueron los principios más frecuentemente encontrados. Los psicoterapeutas parecen tener una mayor preocupación por las relaciones interpersonales y están menos vinculados a la responsabilidad social.
Palabras clave: Psicoterapia; Psicología; Códigos éticos; Práctica profesional
INTRODUCTION
Psychotherapy is one of the oldest structured interventions for persons with mental disorders. It emerged as a model of therapies focused on behavior or meaning when there were not yet effective biological psychiatric interventions. Psychotherapy is born before psychology as an autonomous profession (Buchanan, 2003). However, today it is traditionally practiced by psychiatrists and psychologists, despite some authors arguing for the autonomy of psychotherapy as a profession (Sherman, 2005).
The concept of profession, in general, was developed over time. The first occupations that held the status of profession were theology, medicine, and law, followed by architecture and engineering. The second half of the twentieth century brought an explosion in the number of activities claiming the status of profession (Sinclair et al., 1996). The current definition focuses on the idea of a paid activity with a high degree of training to serve the public. Therefore, it implies the notion of “professing” principles and values1 (Ricou et al., 2017, 2019; European Federation of Psychologists’ Associations [EFPA], 2023). Training and peer supervision and making decisions based on professional principles and values will be the core of professional activity, and its regulation will be a central condition. Hence, the need for a code of ethics, forming a community that can regulate access to the profession, train new members, socialize them with professional attitudes, values, and practices, regulate and monitor their activity, and develops knowledge in the area (Seit & O’Neill, 1996). This community will have to be constituted mainly by the professionals themselves, the only ones able to carry out these tasks in a way that is adequate to the high level of performance that is naturally expected by a professional (Ricou et al., 2017).
Ethics Codes should be based on principles and values (Korkut, 2010), functioning as an educational tool and helping professionals solve dilemmas, even if they can provide a basis for sanctions. Thus, it seems clear that a code of ethics will be an indispensable tool for any profession, its members, future professionals, and the population they serve.
Although psychotherapy is practiced mainly, even if not solely in some countries, by psychologists and psychiatrists2 with their own code of ethics, there are codes of ethics developed by psychotherapy societies (e.g., Association for Family Therapy and Systemic Practice; Canadian Counseling and Psychotherapy Association; World Council for Psychotherapy). One question that remains is whether a psychologist or psychiatrist should guide their practice by its ethical principles or by those developed by the psychotherapy society to which it belongs and where they have specific training.
The model proposed by Tom Beauchamp and James Childress (1994), and the existence of a Universal Declaration of Ethical Principles for Psychologists (Gauthier, 2008) assumes that there are general principles common to all health professionals. This understanding implies the recognition that these professions have a common identity and that this identity is naturally based on their general ethical principles and the standards that result from them. In the same way, the Convention on Human Rights and Biomedicine propose that any intervention in the health field must be carried out with higher professionals’ obligations and standards (Council of Europe [CE], 1997).
It is important to know if psychotherapists should guide their practice according to the general principles and standards of their profession — medicine if they are psychiatrists or psychology if that is the case — or from the principles of the societies to which they belong. Both options have challenges. The first case would imply accepting that a psychiatrist-psychotherapist is different from a psychologist-psychotherapist. Perhaps the psychiatrist-psychotherapist would defend a more medical model of psychotherapy (World Psychiatrist Association [WPA], 2011) and the psychologist-psychotherapist a more contextual model (Wampold, 2001). In this case, we would interpret the same intervention model differently. The second alternative would create the space for developing psychotherapy as an autonomous profession, since psychotherapists would have their own professional identity. The fundamental question about this hypothesis is whether the general training of a psychotherapist, which is not also a psychiatrist or psychologist, is sufficient.
It is not the purpose of this article to answer the two previous questions, at least in a direct way. The authors decided to explore a third way. Considering that no profession can be regulated without a code of ethics with clear rules governing its exercise, it is important to explore and understand the potential differences between the ethical principles of psychotherapy and the principles of a profession like psychiatry or psychology.
In this study, we explore if there are any differences between the ethical principles of psychotherapy and the principles of psychologists and psychiatrists, considering as reference three documents — the Universal Declaration of Ethical Principles for Psychologists (Gauthier, 2008), the EFPA Meta-Code (EFPA, 2005) and the Madrid Declaration on Ethical Standards for Psychiatric Practice (WPA, 2011). The goal is to analyze existing psychotherapy ethics codes using, as a reference, two documents about international principles of psychology and one for psychiatry. The relevance of the present study comes from the absence of an integrative declaration of ethical principles for psychotherapists. Following the procedures of Janel Gauthier (2008) and Ricou (2014) regarding the ethical principles for Psychologists, we analyze the ethics codes of psychotherapy to extract the main ethical principles.
MATERIALS AND METHODS
Procedures
Codes were identified using a bottom-up approach. The search was conducted with Google’s search engine in four languages: English, French, Spanish, and Portuguese, thus covering four of the six most spoken languages in the world. The search was restricted to pdf or doc files to ensure that searched web pages constituted official documents. Given the extensive results found in such a broad search, exact phrases were used. The chosen formulation was “code of ethics” (or code d’éthique, in French, código de ética, in Spanish and Portuguese) or “ethics code” (code de déontologie, in French, código deontológico, in Spanish and Portuguese). Since Portuguese and Spanish share the same keywords, we used Google language tools to conduct individual searches. This choice increased the number of codes selected by Google. The search string used on Google was: psychotherapy “code of ethics” OR “ethics code” AND (filetype:pdf OR filetype:doc).
Figure 1 presents the analysis flowchart. The initial Google entries represent the number of identified documents using the search expression. The final Google entries represent the actual number of entries accessed by analyzing all the search findings. In the initial screening, codes of ethics adopted by psychotherapy associations were included. Informal documents or outdated links were excluded.
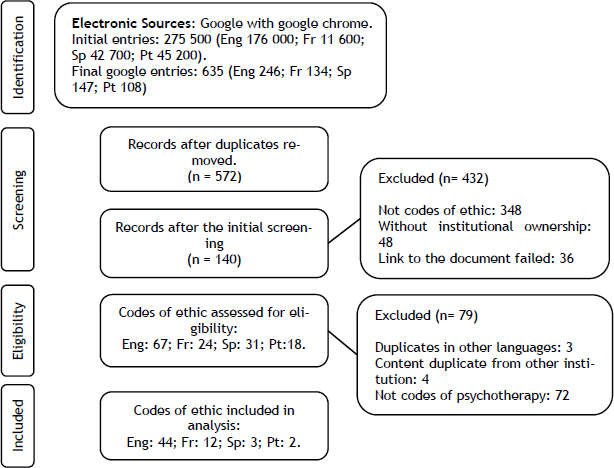
Figure 1. Systematic search flow chart
Data Analysis
The analysis aimed to identify the presence or absence of general and specific principles of the Meta-Code of EFPA (EFPA, 2005) and the Universal Declaration of Ethical Principles for Psychologists (Gauthier, 2008). The Meta-Code of EFPA (EFPA, 2005) is separated into four general principles (i.e., respect for a persons’ rights and dignity, competence, responsibility and integrity) and into 18 dimensions (i.e., privacy and confidentiality, informed consent and freedom of consent, self-determination, ethical awareness, limits of competence, limitations of procedures, continuing development, incapability, promotion of high standards, avoidance of harm, continuity of care, extended responsibility, resolving dilemmas, recognition of professional limitations, honesty and accuracy, straightforwardness and openness, conflict of interests and exploitation, actions of colleagues). The Universal Declaration of Ethical Principles for Psychologists describes and articulates five general principles and related values (respect for the dignity of persons and peoples; competence; caring for the well-being of persons and peoples; integrity; professional and scientific responsibilities to society) (Gauthier, 2008). We used a Meta-Code since it is a general set of principles that apply to several European contexts and cultures, and the Universal Declaration of Ethical Principles for Psychologists because of the generic set of ethical principles and the common moral framework that guides psychologists worldwide. We also used the Madrid Declaration on Ethical Standards for Psychiatric Practice because it is the reference document for the ethical principles for psychiatry practice worldwide (WPA, 2011). Madrid Declaration on Ethical Standards for Psychiatric Practice comprises seven ethical principles that should govern the conduct of psychiatrists, guidelines concerning specific situations, and four additional specific ethical guidelines. The specific guidelines concern: the ethics of psychotherapy in medicine, conflict of interests in relationships with industry, conflicts arising with third parties, boundaries, and trust with patients (WPA, 2011). The categories used in the present analysis were defined from Meta-Code, Universal Ethical Principles, and the Madrid Declaration on Ethical Standards for Psychiatric Practice. We compared the content of ethical principles of the psychology codes and the Madrid Declaration on Ethical Standards for Psychiatric Practice and eliminated those that repeated or had the same meaning. The remaining ones were maintained or renamed and constitute the categorical principles for the analysis.
The analysis sought to identify the categorical principles defined for this study (see Appendix A). Due to the organizational differences across ethical codes, each principle of psychotherapy codes did not have to be exactly equal to our categorical principles. They must be consistent with the content of the categorical principles defined by the Meta-Code, Universal Declaration of Ethical Principles for Psychologists, and Madrid Declaration. For example, the ethics code of the Association for Dance Movement Psychotherapy (UK) contains a statement about the exploitation of the professional relationship under the domain — the best interests of clients. In our categorical principles, this is in agreement with the specific principle of avoiding conflict of interests and was coded under this principle. We did not consider the statements that did not correspond to any content of our categorical principles. For this reason, the analysis constituted a content analysis and followed a consensus approach. Two of the researchers conducted the analysis. When disagreements occurred, those were discussed with the first author, who assisted in reaching a decision.
RESULTS
After applying the excluded criteria, 61 codes of ethics of psychotherapy were included in the content analysis (see Appendix B). We found 44 ethical codes in English, two in Portuguese, three in Spanish, and 12 ethics codes in French, distributed by 17 countries. As presented in Table 1, the majority of ethical codes were from the United Kingdom (n = 12), the next from France (n = 9), and seven from Australia and Ireland (n = 7).
Country |
n |
% |
Australia |
7 |
11.5 |
Australia/New Zealand |
4 |
6.6 |
Brazil |
1 |
1.6 |
Canada |
6 |
9.8 |
France |
9 |
14.8 |
Germany |
1 |
1.6 |
Ireland |
7 |
11.5 |
Mexico |
1 |
1.6 |
Netherlands |
1 |
1.6 |
New Zealand |
1 |
1.6 |
Portugal |
1 |
1.6 |
South Africa |
1 |
1.6 |
Switzerland |
1 |
1.6 |
United Kingdom |
12 |
19.7 |
Uruguay |
1 |
1.6 |
United States of America |
4 |
6.6 |
Venezuela |
1 |
1.6 |
Missing |
2 |
3.3 |
Table 1. Psychotherapy Ethical Codes Found by Country
Psychotherapy ethical codes were coded according to their organization. Ethical codes were differentiated according to the presence or absence of general principles. We found 33 ethical codes that presented well-defined general principles.
The results of the content analysis are presented in Table 2. The principles with greater frequency in ethical codes of psychotherapy were confidentiality (n = 60), competence (n = 60), integrity (n = 58), honesty and accuracy (n = 57), developing and maintaining competence (n = 56), and competence awareness (n = 55). The less frequent were promoting client self-determination (n = 12), extended responsibility (n = 21), social responsibility (n = 30), and ethical awareness (n = 30).
Principles |
Frequency |
% |
Confidentiality |
60 |
98.4 |
Competence |
60 |
98.4 |
Integrity |
58 |
95.1 |
Honesty and accuracy |
57 |
93.4 |
Developing and maintaining competence |
56 |
91.8 |
Competence awareness |
55 |
90.2 |
Respect for the person’s rights and dignity |
53 |
86.9 |
Responsibility |
49 |
80.3 |
Professional responsibility |
49 |
80.3 |
Justice |
44 |
72.1 |
Respect the client and people’s self-determination |
39 |
63.9 |
Informed Consent |
39 |
63.9 |
Avoiding conflicts of interest |
38 |
62.3 |
Non-maleficence |
36 |
59.0 |
Actions of colleagues |
36 |
59.0 |
Beneficence |
34 |
55.7 |
Continuity of care |
32 |
52.5 |
Ethical awareness |
30 |
49.2 |
Social responsibility |
30 |
49.2 |
Extended responsibility |
21 |
34.4 |
Promoting client self-determination |
12 |
19.7 |
Table 2. Percentage of Principles Presence adapted from Meta-Code, Universal ethical principles, and Madrid Declaration
DISCUSSION
In analyzing the results of the codes identified in our search, we intend to highlight the most common principles in all ethics codes of psychotherapy. In the same way, we analyzed the principles with less frequency. The more frequent principles are confidentiality, competence, integrity, honesty, and accuracy, developing and maintaining competence and competence awareness, all with a percentage superior to 90%. On the other hand, the least common are: promoting client self-determination with 19.7%, extended responsibility with 34.4%, and social responsibility and ethical awareness with 49.2%, all below 50%.
Confidentiality is one of the core values in interventions where the relationship is central (Ricou et al., 2019). Trust is fundamental to a relationship. There can be no confidence if there is no privacy (Beauchamp & Childress, 1994), which places the principle of confidentiality as one of the central points in psychological intervention, psychiatry, and psychotherapy. In fact, trust is a common instrument of intervention in psychology, psychiatry, and psychotherapy.
Competence, maintaining competence, and competence awareness are related to the professional training aspect (Ricou et al., 2017) and, therefore, the technical dimension of the intervention. Training in psychotherapy is usually very demanding, with a long period of supervised practice (Wampold, 2001). So, competence is taken very seriously in psychotherapy.
Finally, integrity, honesty, and accuracy are principles associated with the promotion of professional practice (Ricou et al., 2017). Integrity points to the promotion of values such as honesty and congruence, avoiding conflicts of interest that may arise. Psychotherapy is an activity where the psychotherapist and client work alone and together. The psychotherapist usually plays a highly significant role in the client’s life due to their vulnerability and the importance of the relationship established. Therefore, the psychotherapist has a considerable responsibility, and it is fundamental to promote the integrity of their practice according to the principles of their activity.
Concerning the principles less represented in the psychotherapy codes, “promoting self-determination” is the less mentioned. Regarding respect for self-determination or autonomy, codes of psychotherapy are rich concerning this reference. The difference seems to be precisely in the issue of promotion. Psychology is not limited to intervening with people with a problem or difficulty. The objectives of psychological intervention are also put in the development of skills, as stated in the Positive psychology principles (Seligman & Csikszentmihalyi, 2014) and the promotion of self-knowledge. The reduced frequency of this principle in the psychotherapy codes (19.7%) may indicate a clear difference at this level, suggesting a tendency to value the medical model focused on a disease or problem. Similarly, we cannot find any reference to it in the Madrid Declaration for psychiatric practice. Psychotherapy was primarily developed as a response to people with mental disorders in the medical field. It has already been mentioned that psychotherapy emerged before psychology and was associated with medicine, so it was designed as a treatment at this level. The development of psychology, especially in its clinical dimension, seems to have been done much from adopting intervention models developed in psychotherapy (Buchanan, 2003). On the other hand, psychotherapy models have undergone significant development thanks to psychology. Perhaps this is why the questions related to the medical and contextual models of psychotherapy are raised (Wampold, 2001). This dispute focuses very much on questioning whether the technique itself would have a therapeutic effect following the intervention, functioning as a medical treatment, or whether it was the common factors of the different psychotherapeutic models to be responsible for the good outcomes of psychotherapy. Regardless of the complexity of the answer to this question, we can consider that the low reference of this principle, characteristic of psychology and psychological intervention, seems to point towards an approach to the medical model. The valorization of respect for autonomy points to the importance of client involvement in the psychotherapeutic intervention. However, the objectives will not be so much for promoting autonomy as for correcting the problem itself.
The fact that it coincides only with 34.4% of extended responsibility seems to underline yet another important difference between psychotherapy and psychological and psychiatry intervention. This principle is related to the professional’s responsibility for the intervention of all other agents who work with them, whether employees or other professionals with whom he can work as a team. The slightest frequency of this principle may suggest that psychotherapists work more often alone with their clients and less often framed in teams as clinical psychologists and psychiatrists. The idea of psychotherapeutic intervention is significantly associated with the intervention between client and psychotherapist, with no others involved, except for an administrative employee or group interventions. This difference may reflect the broader scope of psychological and psychiatric interventions.
The same argument can be used for social responsibility. Any socially recognized profession must contribute to the common good (Beauchamp & Childress, 1994). However, in the activities connected with health and the promotion of individual well-being, this common good is primarily attained from the individual benefit (CE, 1997). That is, if people are healthy and well, society, in general, will benefit from it. For this reason, social responsibility is not usually one of the central principles of these activities. However, there are frequent dilemmas between the individual interest and the common good, so it is important that professionals, on a case-by-case basis, can reflect on the values involved and make the decisions that they consider most appropriate for this purpose. The fact that psychotherapy values social responsibility less can indicate the individual’s greater value in the context of psychotherapeutic intervention. There seems to be a greater focus on the quality of the intervention and its results on the individual than on the social impact of the same intervention.
The codes of ethics of psychotherapy seem to be focused on promoting more technical dimensions. The most valued principles seem to be the ones that protect and promote the results of the intervention, in the sense of correcting a particular symptom or problem. 45.9% of the psychotherapy codes in the present research do not stem from General Principles. Those are usually aspirational principles designed to help professionals in decision-making (Ricou et al., 2017). These results can point to a more normative code organization, pointing to a technical dimension of psychotherapy rather than a professional one. The same can be said about the lower frequency of the ethical awareness principle. It may suggest that the technical dimension is more important than the professional one for a psychotherapist. Psychology and psychiatry, due to the greater scope of their interventions, will have a broader spectrum of action, namely, assuming a more significant interplay between other, more comprehensive social values.
Psychotherapy is an activity traditionally carried out by psychologists and psychiatrists. Therefore, it will be associated with the objectives of psychological and psychiatric intervention, which raises the question of what these may or may not have in common. The psychiatrist is a physician with a significantly different background from the psychologist. This difference leaves the question of whether a psychotherapist-psychiatrist or psychotherapist-psychologist will have the same professional practice even though they are different professionals. It is similar to questioning whether psychologists or psychiatrists continue to perform their professions or become psychotherapists when practicing psychotherapy.
The ethics meta-code of the European Federation of Psychologists’ Associations (EFPA, 2005), the Universal Principles of Psychologists (Gauthier, 2008), and the Madrid Declaration (WPA, 2011) aim to affirm psychology and psychiatry as professional activities with common professional principles regardless the country where they are practiced. In the same professional activity, the goals and the way of achieving those goals are expected to be similar. Ethical principles are intended to guide professionals in decision-making to achieve professional goals (EFPA, 2005).
Transnationally, the Madrid Declaration (WPA, 2011), for psychiatry, has its chapter for psychotherapy. There are three emergent central principles: implying informed consent, integrity, and confidentiality, plus another principle that calls attention to the fact that psychiatric intervention is not only psychotherapeutic. It should also be pharmacological. It seems a clear appeal to professionals that reminds them of their primary condition as psychiatrists, not psychotherapists. If this is true, a medical psychotherapist will first be a physician and only then a psychotherapist and should guide their practice by the physicians’ code of ethics. Psychotherapy will be considered just one of the intervention methods for the psychiatrist. The same is not valid for clinical psychologists, where psychotherapy may be confused with psychological intervention. In fact, it is not easy to distinguish psychotherapy from psychological intervention. Therefore, it was interesting to understand, in future research, the differences between the codes of ethics of psychotherapy and psychology. In addition, explain whether psychologists and psychiatrists should guide their practice based on ethical principles of professional associations (psychology and medicine) or those developed by a psychotherapy association.
In conclusion, we can suggest that psychotherapists seem concerned with their training and attach importance to supervision. Furthermore, throughout the analysis of the ethical codes, it is possible to observe a concern in all dimensions that contribute to the success of an intervention based on interpersonal relationships, such as privacy, informed consent, competence, and integrity, in the sense of correcting a particular symptom or problem. Due to the greater scope of its interventions and the fact that it is not an activity primarily centered on a therapeutic dimension, psychology will have a broader spectrum of action, assuming a greater interplay between other, more comprehensive social values. After these results, it is possible to argue that psychotherapy practice should be integrated into broader activities like psychology and psychiatry, even if, in the case of psychiatry, it would be, most of the time, integrated with other medical treatments.
APPENDIX A. CATEGORICAL PRINCIPLES WITHIN META-CODE OF EFPA AND THE UNIVERSAL DECLARATION OF ETHICAL PRINCIPLES FOR PSYCHOLOGISTS
General Principles |
Specific Principles |
Content of Ethical Principals |
Respect for persons rights and dignity |
Respect the client and people self-determination |
a) Respect for the unique worth and inherent dignity of all human beings; b) respect for the diversity among persons and peoples; c) respect for the customs and beliefs of cultures, to be limited only when a custom or a belief seriously contravenes the principle of respect for the dignity of persons or peoples or causes serious harm to their well-being. |
Promoting client self-determination |
|
|
Justice |
a) Fairness and justice in the treatment of persons and peoples; b) avoidance of practices which are the result of unfair bias and may lead to unjust discrimination. |
|
Informed Consent |
a) Free and informed consent, as culturally defined and relevant for individuals, families, groups, and communities. |
|
Confidentiality |
a) Privacy for individuals, families, groups, and communities; b) protection of confidentiality of personal information, as culturally defined and relevant for individuals, families, groups, and communities. |
|
Competence |
Developing and maintaining competence |
a) Obligation to continue professional development. |
Competence awareness |
a) Self-knowledge regarding how their own values, attitudes, experiences, and social contexts influence their actions, interpretations, choices, and recommendations; b) respect for the ability of individuals, families, groups, and communities to make decisions for themselves and to care for themselves and each other; c) limits of competence; d) correcting or offsetting harmful effects that have occurred as a result of their activities. |
|
Ethical awareness |
a) Obligation to have a good knowledge of ethics, including the Ethical Code, and the integration of ethical issues with professional practice. |
|
Beneficence |
a) Active concern for the well-being of individuals, families, groups, and communities; b) maximizing benefits and minimizing potential harm to individuals, families, groups, and communities. |
|
Non-maleficence |
a) Taking care to do no harm to individuals, families, groups, and communities. |
|
Integrity |
Honesty and accuracy |
a) General obligation to provide information and avoid deception; b) maximizing impartiality and minimizing biases; c) not exploiting persons or peoples for personal, professional, or financial gain. |
Avoiding conflicts of interest |
a) Awareness of the problems which may lead to a conflict of interests, or exploitation of a client and the obligation not to exploit the professional relationship. |
|
Actions of colleagues |
a) Obligation to give a reasonable critique of the professional actions of colleagues, and to take action to inform colleagues and, if appropriate, the relevant professional associations and authorities, if there is a question of unethical action. |
|
Responsibility |
Social responsibility |
a) The discipline’s responsibility to increase scientific and professional knowledge in ways that allow the promotion of the well-being of society and all its members; b) the discipline’s responsibility to use psychological knowledge for beneficial purposes and to protect such knowledge from being misused, used incompetently, or made useless; c) the discipline’s responsibility to conduct its affairs in ways that are ethical and consistent with the promotion of the well-being of society and all its members; d) the discipline’s responsibility to promote the highest ethical ideals in the scientific, professional and educational activities of its members. |
Professional responsibility |
a) Responsibility for the quality and consequences of the psychologist’s professional actions. |
|
Continuity of care |
a) Responsibility for the necessary continuity of professional care of clients, including collaboration with other professionals and appropriate action when a psychologist must suspend or terminate involvement; b) responsibility towards a client, which exists after the formal termination of the professional relationship. |
|
Extended responsibility |
a) Assumption of general responsibility for the scientific and professional activities, including ethical standards, of employees, assistants, supervisors and students. |
APPENDIX B. CODES INCLUDED IN THE ANALYSIS
Affiliation |
Model |
Country |
American Association for Marriage and Family Therapy |
Family or Systemic Therapy |
USA |
Association for Dance Movement Psychotherapy UK |
Relational Psychotherapy |
UK |
American Dance Therapy Association |
Relational Psychotherapy |
USA |
Association for Family Therapy and Systemic Practice |
Family or Systemic Therapy |
UK |
Australian and New Zealand Arts Therapy Association |
Art Therapy |
Australia/New Zealand |
Association for Psychoanalysis and Psychotherapy in Ireland |
Psychoanalytic or Psychodynamic Therapy |
Ireland |
Australian Radix Body Centered Psychotherapy Association |
Somatic Psychotherapy |
Australia |
Association of Soul Centered Psychotherapists |
Relational Psychotherapy |
Australia |
Australian Somatic Psychotherapy Association |
Somatic Psychotherapy |
Australia |
Australian and New Zealand Association of Psychotherapists |
Psychoanalytic Psychotherapy |
Australia/New Zealand |
Australian Society of Clinical Hypnotherapists |
Hypnotherapy |
Australia |
British Association of Art Therapists |
Art Therapy |
UK |
BeeLeaf Institute for Contemporary Psychotherapy |
Contemporary Psychotherapy |
UK |
California Association of Marriage and Family Therapists |
Family or Systemic Therapy |
California |
Canadian Counselling and Psychotherapy Association |
|
Canada |
Clinical Hypnotherapy and Psychotherapy Association |
Hypnotherapy |
Ireland |
College of Registered Psychotherapists of Ontario |
|
Canada |
Equine Assisted Psychotherapy and Personal Development |
Equine Assisted Psychotherapy |
USA |
European Association for Gestalt Therapy |
Gestalt Therapy |
Netherlands |
European Association for Transactional Analysis |
Transactional Analysis |
Germany |
Federation of Associations of Counselling Therapists – Alberta |
|
Canada |
Feminist Therapy Institute |
Humanistic |
Missing |
Gestalt Australia and New Zealand |
Gestalt Therapy |
Australia/New Zealand |
Hakomi Institute |
Experiential Psychotherapy |
USA |
Irish Association for Counselling and Psychotherapy |
|
Ireland |
Irish Association of Humanistic and Integrative Psychotherapy |
Humanistic and Integrative Psychotherapy |
Ireland |
Irish Association for Play Therapy and Psychotherapy |
|
Ireland |
Institute of Clinical Hypnotherapy & Psychotherapy Graduates Association |
Hypnotherapy |
Ireland |
Metanoia Institute |
|
UK |
National Association for Pastoral Counselling & Psychotherapy |
|
Ireland |
Northern Guild Psychotherapy & Counselling |
|
UK |
NSW Institute of Psychoanalytic Psychotherapy |
Psychoanalytic Psychotherapy |
Australia |
New Zealand Association of Psychotherapists |
|
New Zealand |
Ontario Association of Consultants, Counsellors, Psychometrists and Psychotherapists |
|
Canada |
Professional Association of Christian Counsellors and Psychotherapists |
|
Canada |
Psychotherapy & Counselling Federation of Australia |
|
Australia |
Psychoanalytic Psychotherapy Association of Australasia |
Psychoanalytic Psychotherapy |
Australia/New Zealand |
South African Psychoanalytic Confederation |
Psychoanalytic Psychotherapy |
South Africa |
The Sherwood Psychotherapy Training Institute |
Gestalt Psychotherapy |
UK |
The Bowlby Centre |
Psychoanalytic Psychotherapy T |
UK |
College for Sexual and Relationship Psychotherapy |
|
UK |
UK Council for Psychotherapy |
|
UK |
British Psychodrama Association |
Psychodrama and Sociodrama |
UK |
Victorian Association of Psychoanalytic Psychotherapists |
Psychoanalytic Psychotherapists |
Australia |
West Midlands Institute of Psychotherapy |
Psychoanalytic Psychotherapy |
UK |
Associação de Psicanálise Relacional |
Psychoanalysis |
PT |
Ordem Nacional dos Psicanalistas |
|
Brazil |
Federación Latinoamericana de Sociedades de Sexologia Y Educación Sexual |
|
Uruguay |
Associación Venezuelana de Psicoterapia |
|
Venezuela |
Asociación Mexicana de Orientación Psicológica y Psicoterapia |
|
México |
Analyse Psycho-organique de l’EFAPO |
Psychoanalysis |
France |
Association Internationale de Somathotérapie |
Somatanalyse |
France |
Institut de Sophrologie de Rennes |
Phenomenological |
France |
Fédération Française de Psychothérapie |
|
France |
Association Française de Psychothérapie dans l’Approche Centrée sur la Personne A.C.P |
Humanistic |
France |
Fédération Française De Sophrologie |
Phenomenological |
France |
l’Association Professionnelle Suisse des Art-Thérapeutes |
Art Therapy |
Suisse |
Fédération Française des Art Thérapeutes |
Art Therapy |
France |
Association des Art Thérapeutes du Québec |
Art Therapy |
Canada |
Institut Francais de Formation en Sexothérapie |
Humanistic and Holistic |
France |
Syndicat National des Praticiens en Psychothérapie Relationnelle et Psychanalyse |
Relational Psychotherapy |
France |
European Association For Psychotherapy |
|
Missing |
REFERENCES
Beauchamp, Tom & Childress, James (1994). Principles of biomedical ethics. Oxford University Press.
Buchanan, Roderick D. (2003). Legislative warriors: American psychiatrists, psychologists, and competing claims over psychotherapy in the 1950s. Journal of History of the Behavioral Sciences, 39(3), 225–249. https://doi.org/10.1002/jhbs.10113
Council of Europe (1997). Convention for the protection of human rights and dignity of the human being with regard to the application of biology and medicine: Convention on human rights and biomedicine. https://rm.coe.int/168007cf98
European Federation of Psychologists’ Association (2005). Meta-code of ethics. http://ethics.efpa.eu/metaand-model-code/meta-code/
European Federation of Psychologists’ Association (2023). Glossary: Definition of terms used in EFPA Board of Ethics documents and position papers. https://www.efpa.eu/glossary
Gauthier, Janel (2008). The draft universal declaration of ethical principles for psychologists: A revised version. International Association of Applied Psychology/Newsletter, 20(2), 45-49.
Korkut, Yesim (2010). Developing a national code of ethics in psychology in Turkey. Balancing international ethical systems guides with a nation’s unique culture. Ethics and Behavior, 20(3-4), 288-296. https://doi.org/10.1080/10508421003799057
Ricou, Miguel; Sá, Eduardo & Nunes, Rui (2017). Ethical principles of Portuguese psychologists. A universal approach. Journal of Medicine and Philosophy, 42(2), 199-213. https://doi.org/10.1093/jmp/jhw066
Ricou, Miguel; Sá, Eduardo & Nunes, Rui (2019). The ethical principles of the Portuguese psychologists: An empirical approach. Journal of Medicine and Philosophy, 44, 109-131. https://doi.org/10.1093/jmp/jhy036
Seit, Joanne & O’Neill, Patrick (1996). Ethical decision-making and the code of ethics of the Canadian Psychological Association. Canadian Psychology, 37, 23-30. https://doi.org/10.1037/0708-5591.37.1.23
Seligman, Martin E. P. & Csikszentmihalyi, Mihaly. (2014). Positive psychology: An introduction. In Mihaly Csikszentmihalyi (Ed.), Flow and the Foundations of Positive Psychology (pp. 279-298). Springer. https://link.springer.com/content/pdf/bfm%3A978-94-017-9088-8%2F1.pdf
Sherman, Eric (2005). Notes from the margins: The gay analyst’s subjectivity in the treatment setting. The Analytical Press, Inc, Publishers.
Sinclair, Carol; Simon, Norma P. & Pettifor, Jean L. (1996). The history of ethical codes and licensure. In Larry J. Bass & Stephen. T. DeMers (Eds.), Professional conduct and discipline in psychology (pp. 1-16). American Psychological Association.
Wampold, Bruce E. (2001). The great psychotherapy debate: Models, methods, and findings. Lawrence Erlbaum Associates Publishers.
World Psychiatrist Association (2011). Madrid declaration on ethical standards for psychiatric practice. http://www.wpanet.org/current-madrid-declaration?lang=de

MIGUEL RICOU
Psychologist, PhD in Clinical Psychology. President of the Clinical and Health Psychology Division of the Portuguese Order of Psychologists. Co-Convener of the Board of Ethics of EFPA – Portuguese Representative. Faculty of Medicine of Oporto University, Portugal. Member of CINTESIS@RISE - Center for Health Technology and Services Research.
mricou@med.up.pt
https://orcid.org/0000-0002-8190-9587
DAVID D. NETO
Is an assistant professor at ISPA – Instituto Universitário. He concluded his doctoral degree in 2011, jointly awarded by the University of Lisbon and the University of Sheffield. He has published several papers and edited books in psychotherapy research, clinical and health psychology, and psychopathology.
dneto@ispa.pt
https://orcid.org/0000-0002-3129-262X
ANA N. SILVA
PhD, C.Psych. Guest Assistant Professor at the Department of Cognitive Behavioral and Integrative Psychology of the Faculty of Psychology of the University of Lisbon, Portugal. Researcher at CICPSI – Centro de Investigação em Ciências Psicológicas.
acsilva@psicologia.ulisboa.pt
https://orcid.org/0000-0001-7125-716X
SÍLVIA MARINA
PhD, Psychologist. Researcher at CINTESIS@RISE - Center for Health Technology and Services Research. Member of the committee of ethics of the Portuguese Order of Psychologists. Her main research is in psychological intervention, end-of-life decision making and the role of psychologists in euthanasia/assisted suicide.
silviamarina@outlook.com
https://orcid.org/0000-0003-4808-9000
FUNDING
This article was supported by National Funds through FCT - Fundação para a Ciência e a Tecnologia, I.P., within CINTESIS, R&D Unit (reference UIDB/4255/2020).
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any com-mercial or financial relationships that could be construed as a potential conflict of interest.
AUTHOR CONTRIBUTIONS
Miguel Ricou contributed to the design, interpretation of the data, drafting, and critically revised the article. David Neto contributed to the data collection, draft-ing, and critically revised the article. Ana Silva contributed to data collection, analysis, and interpretation of data and revised the article. Sílvia Marina contribut-ed to data collection, analysis, and interpretation of data and revised the article.
DATA ACCESSIBILITY STATEMENT
The data that support the findings of this study are available from the correspond-ing author, [SM], upon reasonable request.
FORMATO DE CITACIÓN
Ricou, Miguel; Neto, David; Silva, Ana & Marina, Sílvia (2023). Ethical principles in psychotherapy within a broad psychological and medical deontological framework: An international comparison. Quaderns de Psicologia, 25(2), e1867.
https://doi.org/10.5565/rev/qpsicologia.1867
HISTORIA EDITORIAL
Recibido: 30-07-2021
1ª revisión: 07-04-2023
Aceptado: 23-05-2023
Publicado: 30-07-2023
_______________________________
1 In this paper, we use the definition of principles and values proposed by the European Federation of Psychologists’ Associations. Principles represents values that orient and rule the professional conducts. Values are the moral, ethical and belief paradigms of an individual or group determining their actions in daily life (European Federation of Psychologists’ Associations [EFPA], 2023).
2 Some psychotherapy Societies or Associations also accept other professional backgrounds then psychiatrists or psychologists. Nevertheless, in this study we just have included these two professions because they are the most common and universally accepted as psychotherapists.